
Study finds inverse correlation between dietary magnesium intake and peripheral arterial disease

In a recent article published in PLOS One, researchers conducted a cross-sectional study to investigate the association between dietary magnesium intake and peripheral arterial disease (PAD), a chronic atherosclerotic disease primarily affecting the lower extremities.
The study was carried out using deidentified and publicly available data from the National Health and Nutrition Examination Survey (NHANES) survey.
Background
The National Center for Health Statistics (NCHS) conducted the NHANES survey to assess the health of United States (US) citizens through physical examinations, lab tests, and interviews between 1999 and 2004. This data helped the researchers investigate the potential relationship between dietary magnesium intake and various diseases, including PAD.
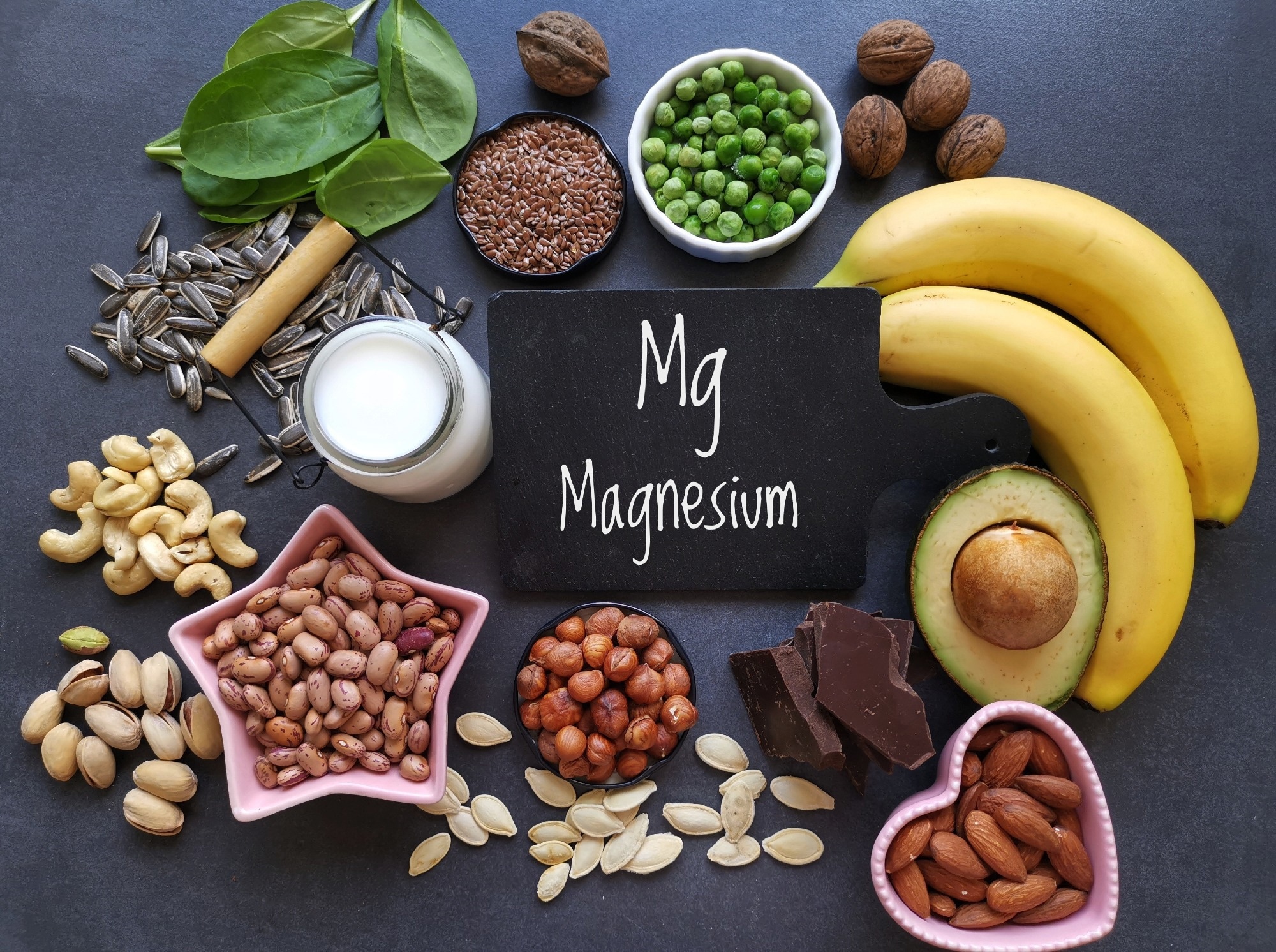
Magnesium is an essential trace element primarily consumed through the diet. It is mainly present in cells and bone, with serum magnesium accounting for a small fraction, which makes assessing serum magnesium levels challenging.
Nonetheless, magnesium plays a crucial role as a physiological regulator of vascular tone. Previous studies have shown that low serum magnesium leads to a metabolic imbalance in patients with diabetes, increasing the risk of PAD.
About the study
In the present study, researchers determined PAD by measuring the ankle-brachial index (ABI), where an ABI of less than 0.9 in at least one ankle (left or right) indicated PAD. Additionally, they measured the systolic blood pressure on both ankles and the brachial artery of either the right or left arm.
The subject-driven 24-hour dietary recall method helped the researchers compile a list of foods/beverages that a person consumed in 24 hours. Then, they used the National Nutrition Standards Reference database to determine each subject's dietary magnesium intake in the past 24 hours.
Further, they divided the dietary magnesium intake into four quartiles, with Q1 to Q4 indicating magnesium intake between ≤179.00mg and >343.00mg.
The study covariates included age, gender, race/ethnicity, education status, and annual family income. The team also determined their body mass index (BMI), smoking status, and comorbidities like hypertension and diabetes. They used an enzymatic assay to determine each subject's triglycerides and cholesterol and the Beckman Coulter MAXM instrument to assess their platelet count.
Finally, the team did weighted statistical analyses on all the NHANES data. They presented continuous variables as mean ± standard error and non-normally distributed variables as median or interquartile range (IQR). Likewise, they presented categorical variables as numbers (percentages).
Results
The researchers performed an ABI test on all NHANES participants aged ≥40, totaling 9,970 individuals. After exclusions for missing covariate and bilateral ABI data, the final analysis sample comprised 5,969 participants. Of these, 409 and 5,560 individuals constituted the PAD and the non-PAD group, respectively.
The median age of the participants in the PAD and non-PAD groups was 68 and 53 years, respectively, further reinforcing the idea that PAD incidence is higher in middle- and old-aged people.
The authors noted an association between the intake of trace minerals, especially magnesium, and the development of PAD. Accordingly, Q1 was associated with a higher PAD incidence, with an odds ratio (OR) of 1.56.
This association remained significant in people of non-white ethnicities, people with no comorbidities, and who never or formerly smoked. Furthermore, the study analysis revealed a possible interaction between dietary magnesium intake and age.
The results also highlighted that the magnesium intake of middle-and old-aged people in the US is below the recommended intake. Subjects without PAD and with PAD, on average, consumed 288.30 mg/d and 244.89 mg/d magnesium daily, both of which were lower than the recommended intake.
Multiple factors increase the PAD risk amid magnesium deficiency. First, magnesium acts as a calcium antagonist; it promotes vasodilatation and blood circulation by increasing peripheral arterial blood flow and reducing vasoconstriction.
Second, magnesium reduces the levels of inflammatory factors, such as C-reactive protein (CRP), tumor necrosis factor-alpha (TNF-α), and interleukin-6 (IL-6). Lastly, It also reduces calcium deposition in the vascular wall and vascular calcification.
Conclusions
Numerous previous studies have explored the link between serum magnesium levels and PAD; however, this is one of the first to investigate the association between PAD and dietary magnesium consumption.
The study used a nationally representative larger sample from the general population, with its results suggesting a significant inverse correlation between PAD risk and dietary magnesium intake. Further prospective studies should validate these findings.
- Wu Z, Ruan Z, Liang G, Wang X, Wu J, & Wang B (2023). Association between dietary magnesium intake and peripheral arterial disease: Results from NHANES 1999–2004. PLOS ONE, 18(8), e0289973. doi: 10.1371/journal.pone.0289973. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0289973
Posted in: Medical Research News | Medical Condition News | Disease/Infection News
Tags: Assay, Blood, Blood Pressure, Body Mass Index, Bone, Calcification, Calcium, Cholesterol, Chronic, C-Reactive Protein, Diabetes, Diet, Education, Interleukin, Interleukin-6, Magnesium, Minerals, Necrosis, Nutrition, Peripheral Arterial Disease, Platelet, Protein, Smoking, Tumor, Tumor Necrosis Factor, Vascular

Written by
Neha Mathur
Neha is a digital marketing professional based in Gurugram, India. She has a Master’s degree from the University of Rajasthan with a specialization in Biotechnology in 2008. She has experience in pre-clinical research as part of her research project in The Department of Toxicology at the prestigious Central Drug Research Institute (CDRI), Lucknow, India. She also holds a certification in C++ programming.