
A cutting-edge MRI technique to detect iron deposits in different brain regions can track declines in thinking, memory and movement in people with Parkinson’s disease, finds a new UCL-led study.
The findings, published in the Journal of Neurology, Neurosurgery, and Psychiatry, suggest that measures of brain iron might eventually help predict which people with Parkinson’s will develop dementia.
“Iron in the brain is of growing interest to people researching neurodegenerative diseases such as Parkinson’s and dementias. As you get older, iron accumulates in the brain, but it’s also linked to the build-up of harmful brain proteins, so we’re starting to find evidence that it could be useful in monitoring disease progression, and potentially even in diagnostics,” said the study’s lead author, Dr. Rimona Weil (UCL Queen Square Institute of Neurology).
The study involved 97 people with Parkinson’s disease, who had been diagnosed within the last 10 years, along with 37 people without the condition, as a control (comparison) group. They were tested for their thinking and memory as well as for their motor function.
Parkinson’s disease is a progressive condition of brain degeneration resulting in tremors, stiffness and slowness of movement. Close to 50% of people with the condition end up developing dementia, but the timing and severity vary substantially.
Currently there are no reliable measures to track Parkinson’s progression in the brain, so clinicians rely on monitoring symptoms. Conventional brain imaging fails to track progression until quite a late stage, when large-scale brain volume loss can be detected.
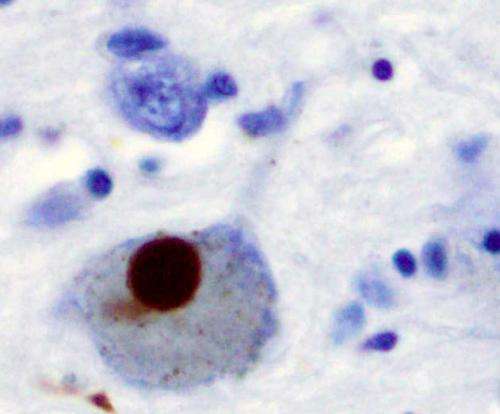
Iron accumulates in people’s brains as part of the normal ageing process, partly due to increased permeability in the blood-brain barrier. Excess iron can have toxic effects leading to proteins being irreversibly modified. Recent studies have found that when proteins linked to Alzheimer’s disease (amyloid and tau, which are also linked to Parkinson’s dementia) build up, iron also accumulates in the affected brain areas.
In the current study, researchers used a new technique, called quantitative susceptibility mapping, to map iron levels in the brain based on MRI (magnetic resonance imaging) scans. They found that iron accumulation in the hippocampus and thalamus brain regions was associated with poor memory and thinking scores. Iron in the putamen brain region was associated with poor movement scores, suggesting a more advanced stage of the disease.
In Parkinson’s disease, the hippocampus and thalamus are known to be associated with thinking and memory, and the putamen with movement scores, so the researchers say it’s very promising that iron deposition was specifically detected in those areas.
The findings suggest that iron deposition could be valuable to track if a treatment is working in a clinical trial, and might eventually be helpful for early diagnosis of Parkinson’s or other neurodegenerative diseases.
Dr. Weil has previously found in a 2019 study that a suite of vision tests may be helpful to predict cognitive decline in Parkinson’s. She and her colleagues hope that further research will determine if the vision tests and iron measures could be helpful to predict which people with dementia are likely to develop dementia.
First author, Ph.D. student George Thomas (UCL Queen Square Institute of Neurology), said: “It’s really promising to see measures like this which can potentially track the varying progression of Parkinson’s disease, as it could help clinicians devise better treatment plans for people based on how their condition manifests.”
Co-author Dr. Julio Acosta-Cabronero (Tenoke Ltd. and Wellcome Centre for Human Neuroimaging, UCL) added: “We were surprised at how well the iron levels measured in different regions of the brain with MRI were correlated with cognitive and motor skills. We hope that brain iron measurement could be useful for a wide range of conditions, such as to gauge dementia severity or to see which brain regions are affected by other movement, neuromuscular and neuroinflammatory disorders, stroke, traumatic brain injury and drug abuse.”
Source: Read Full Article