
Researchers in the United States have developed an alternative messenger RNA (mRNA) delivery platform to the lipid nanoparticles that are currently used in vaccines against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) – the agent that causes coronavirus disease 2019 (COVID-19).
The lipid nanoparticle (LNP) delivery vehicles have inherent immunostimulatory properties that can induce adverse events such as allergic reactions.
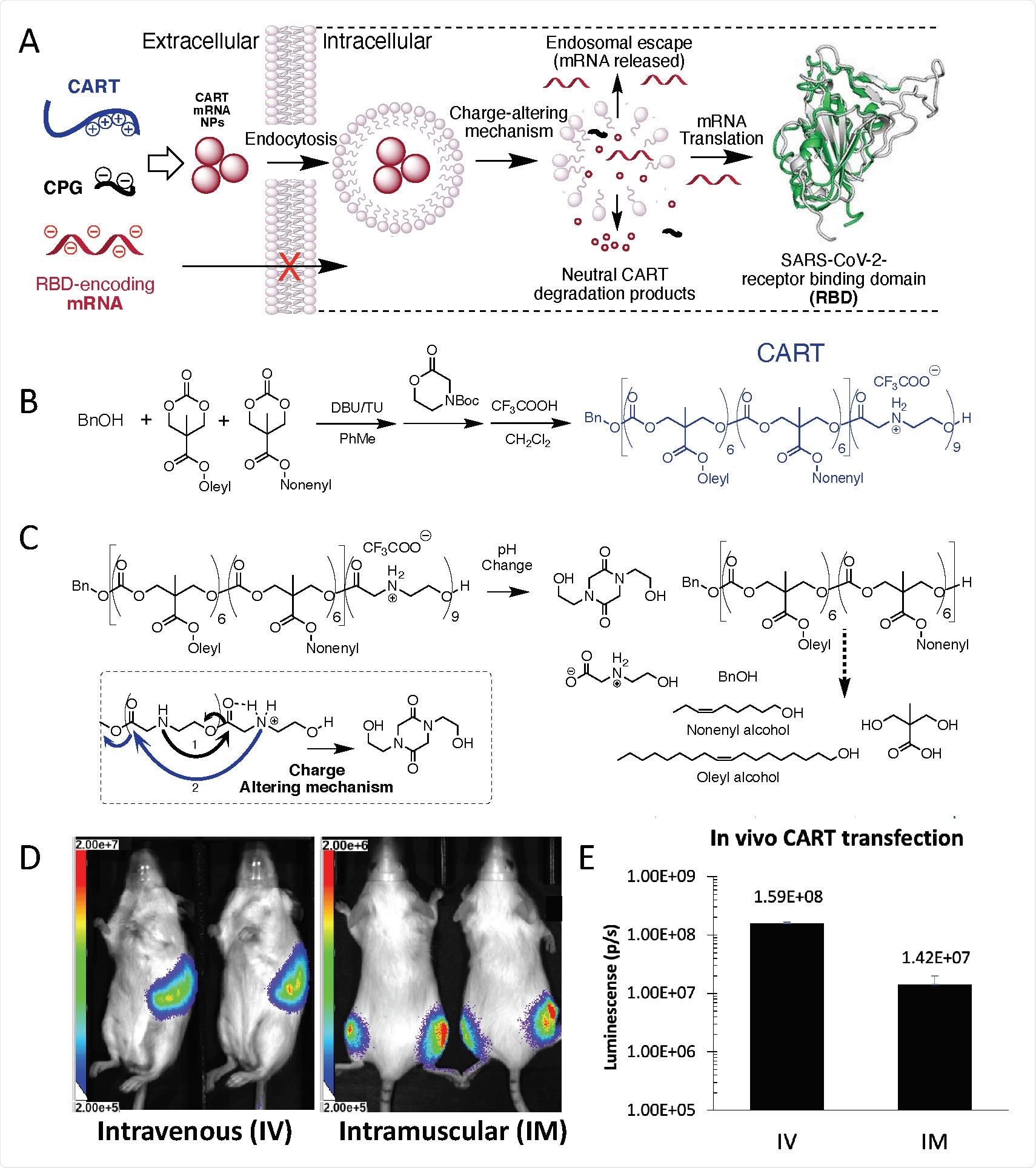
Now, Ronald Levy and colleagues from Stanford University in California have developed an alternative approach that uses a novel delivery vehicle called Charge-Altering Releasable Transporters (CARTs).
“Using these inherently nonimmunogenic vehicles, we are able to tailor the vaccine immunogenicity by the inclusion of co-formulated adjuvants such as oligonucleotides with CpG motifs,” they write.
Mice vaccinated with the mRNA-CART-CpG vaccine developed therapeutically relevant levels of neutralizing antibodies against the receptor-binding domain (RBD) of the SARS-CoV-2 viral sike protein.
This spike protein mediates the initial stage of the infection process by binding to the host cell receptor angiotensin-converting enzyme 2 (ACE2).
The RBD-specific neutralizing antibodies were generated in both the circulation and the lung bronchial fluid of the animals.
The vaccine also elicited strong and long-lasting RBD-specific TH1 T cell responses, including CD4+ and CD8+ T cell memory.
A pre-print version of the paper is available on the bioRxiv* server, while the article undergoes peer review.
mRNA vaccines could address the emergence of new variants
The COVID-19 pandemic has necessitated the rapid development of safe, effective, and scalable vaccines to protect against infection with SARS-CoV-2.
“mRNA vaccines offer flexible and fast design that will allow for subsequent generations of products to address the emergence of new virus variants,” say the researchers.
The currently approved mRNA vaccines are formulated with LNP delivery vehicles. These delivery systems contain ionizable lipids that can induce adverse events. They also contain polyethylene glycol (PEG), which can contribute to allergic reactions.
“One important aspect for the continuous success and refinement of mRNA-based therapeutics in general will be to create access to diverse choices of safe delivery vehicles with varying chemical and biological properties,” says Levy and the team.
The recent emergence of mutations in the SARS-CoV-2 spike RBD that have been shown to mediate escape from vaccine-induced immunity also underscores the urgent need for flexible and rapidly adaptable vaccine platforms.
CARTS are readily producible and scalable oligomers that electrostatically encapsulate mRNA and deliver it into cells.
“In contrast to LNPs, CARTs have no unspecific immunostimulatory effects, which allows more flexibility for vaccine design and the option to choose the appropriate adjuvant to co-deliver with mRNA, rather than relying on the inherent immunogenicity properties of LNPs,” says the team.
What did the researchers do?
Now, Levy and colleagues have developed an mRNA-based vaccine encoding the SARS-CoV-2 spike RBD that is formulated with a highly efficient, non-toxic, PEG-free mRNA delivery CARTs platform and cytidine-phosphate-guanosine (CpG) as an adjuvant.
The CpG adjuvant directly activates plasmacytoid dendritic and B cells, contributing to the induction of both innate and adaptive immune responses.
The team compared the use of this RBD mRNA + CpG-CART platform using a vaccine that did not contain CpG (RBD mRNA-CART) in mice.
Mice vaccinated with RBD mRNA + CpG-CART developed robust RBD-specific immunoglobulin G (IgG) and IgM antibody responses in the circulation just four days following immunization.
The RBD-specific antibody responses in the mice that received CpG consistently exceeded those observed among the mice that did not receive CpG. By day 60, levels of all classes of RBD-specific antibodies were higher in the serum of mice vaccinated with the CpG-containing vaccine.
The CpG-containing vaccine induced higher levels of neutralizing antibodies
Next, the team tested the anti-sera for their ability to inhibit the RBD-ACE2 interaction and to block pseudotyped viral entry into ACE2-expressing cells.
On day 28 following vaccination, the level of neutralizing antibodies was significantly higher in the mice that had received CpG than among the mice that had not.
Anti-sera from the CpG mice also displayed a significantly higher degree of ACE2 blocking and neutralization of pseudotyped virus than anti-sera from the non-CpG mice.
To evaluate the presence of RBD-specific IgGs in the lungs of the animals, the team collected bronchoalveolar lavage (BAL) on day 60 following immunization and performed an ELISA.
RBD-specific IgGs were detected in BAL collected from both the CpG mice and the non-CpG mice.
What about the cellular response?
The RBD mRNA + CpG-CART vaccine also induced strong and long-lasting RBD-specific TH1 T cell responses, including CD4+ and CD8+ T cell memory.
“Remarkably, upon RBD protein restimulation, a defined RBD-specific CD4+ /CD44high/CD134+ and CD4+ /CD44high/TNFa+ activated T cell subset was observed in lung cell suspensions from mice vaccinated with RBD mRNA + CpG-CART,” says Levy and colleagues.
“An alternative mRNA delivery platform”
“Here we demonstrate an effective mRNA vaccination strategy against the clinically relevant RBD antigen of SARS-CoV-2 using an alternative mRNA delivery platform to the clinically used lipid nanoparticles,” say the researchers.
Levy and colleagues point out that CARTs can be readily prepared and formulated with multiple mRNAs in any desired nucleotide combination. Their manufacture also does not require specialized microfluidics instruments.
“Our study demonstrates the potency and flexibility of this mRNA-CART vaccine platform,” concludes the team.
*Important Notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Levy R, et al. An mRNA SARS-CoV-2 vaccine employing a novel delivery vehicle with a TLR-9 agonist induces neutralizing antibodies and T cell memory. bioRxiv, 2021. doi: https://doi.org/10.1101/2021.04.14.439891, https://www.biorxiv.org/content/10.1101/2021.04.14.439891v1
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: ACE2, Angiotensin, Angiotensin-Converting Enzyme 2, Antibodies, Antibody, Antigen, CD4, Cell, Coronavirus, Coronavirus Disease COVID-19, CpG, Enzyme, Gene, Gene Expression, Immunization, Immunoglobulin, in vivo, Lipids, Luciferase, Lungs, Microfluidics, Nanoparticle, Nanoparticles, Nucleotide, Oligonucleotides, Pandemic, Protein, Receptor, Reporter Gene, Respiratory, RNA, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome, Therapeutics, Translation, Vaccine, Virus

Written by
Sally Robertson
Sally first developed an interest in medical communications when she took on the role of Journal Development Editor for BioMed Central (BMC), after having graduated with a degree in biomedical science from Greenwich University.
Source: Read Full Article