
The highly infectious nature of the new coronavirus (SARS-COV-2) has changed social habits throughout the world. Even with vaccinations on the rise, many countries hesitate to allow their residents to return to pre-pandemic activity. Moreover, they continue to demand that infected people isolate themselves for a minimum number of days after the onset of symptoms in a one-size-fits-all manner.
In a new study, a multi-national effort that included researchers at the Institute for Advanced Study of Biology (ASHBi), Kyoto University, Japan, uses a mathematical simulator of the SARS-COV-2 dynamics to demonstrate that the number of days can be reduced for many patients if PCR tests are used.
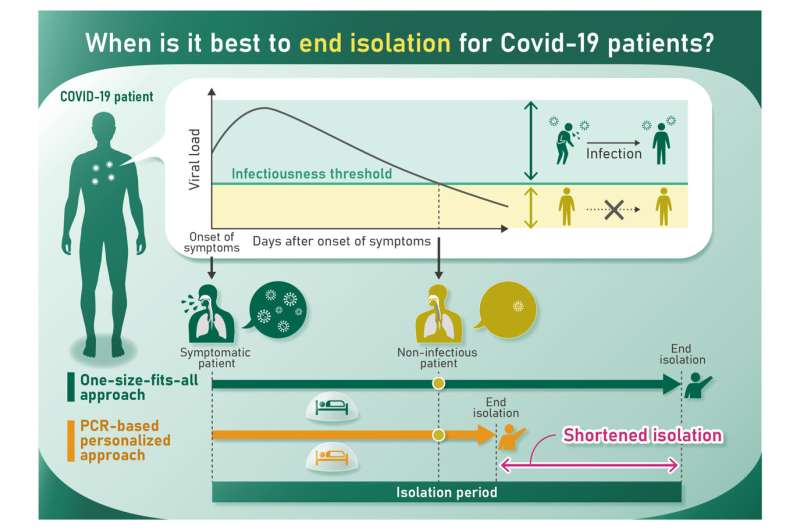
Patient isolation is one of the most effective if not most effective means of preventing the spread of SARS-COV-2. Beginning last year, people had to quickly adapt to weeks-long isolation after testing positive or showing symptoms, but these policies are exhausting societies. To maintain public cooperation, policymakers are seeking guidelines that shorten the isolation period while minimizing the risk of releasing infectious patients.
Dr. Shingo Iwami, an Associate Investigator at ASHBi and author of the study, explains that countries would be wise to consider more personalized decisions to shorten the isolation period.
“Longer isolation periods surely prevent transmission, but also impose substantial burden on isolated patients,” he said. “We found that PCR tests can shorten the isolation period without increasing the risk of further infection.”
PCR tests provide a measure of the viral load in the patient, which is an indicator of infection risk.
To demonstrate the benefits of PCR tests for deciding isolation periods, Iwami and his colleagues, including Keisuke Ejima from Indiana University (United States) and Yong Dam Jeong from Pusan University (South Korea), assessed isolation periods with and without PCR tests using the new simulator. On average, they found that using PCR tests reduced the isolation period by 2 days compared with the one-size-fits-all approach.
“This is not a big surprise,” said Iwami. “The one-size-fits-all approach considers only the symptom onset, but PCR tests provide information on viral load.”
However, he admits that PCR tests may not be feasible everywhere. Because the tests require health professionals, they are costly and must be conducted at designated locations. Thus, a system dependent on PCR tests is more likely to succeed if patients are isolated in dedicated facilities and will be much harder to implement if patients are isolated at home.
With these points in mind, Iwami said that the current guidelines adopted, which depend on clinical and epidemiological data, are overall fairly good.
Source: Read Full Article