
The treatment of blood cancers has dramatically improved in the last five years, thanks to a new class of cancer immunotherapies called CAR-T cell therapy. This therapy—which involves engineering a patient’s own T cells in the lab to kill cancer cells and then infusing them back into the patient—cures about 40% of people with otherwise incurable lymphoma. But others relapse or don’t respond to the treatment at all.
To learn about the molecular mechanisms underlying such different responses, researchers at the Broad Institute of MIT and Harvard, Dana-Farber Cancer Institute, and Massachusetts General Hospital, studied blood samples of patients who received CAR-T therapy. They found molecular markers that indicate how a patient responded to the treatment, and also identified specific types of immune cells that likely contribute to relapse.
The authors say their study, which appears today in Nature Medicine and is part of a Broad and IBM collaboration investigating resistance to cancer treatment, could one day help doctors select the best treatment for their patients and help scientists optimize these therapies to improve response rates.
“Gaining understanding of the T cell phenotypes of CAR-T cells before and after infusion provides us with insight into the basis for why patients do or do not respond to this potentially life-saving therapy,” said Catherine Wu, co-senior author on the study and an institute member at Broad, professor of medicine at Harvard Medical School and Dana-Farber, and staff physician at Dana-Farber and Brigham and Women’s Hospital.
CAR-T collaborations
In their study, the researchers used single-cell RNA-sequencing to analyze gene expression of the patients’ immune cells, tumor cells, and the engineered T cells that were infused into the patients as part of the CAR-T treatment. They generated the largest set of gene expression data from CAR-T cell therapy patients to date, spanning 105 samples collected from 32 patients over the course of treatment. Nicholas Haradhvala, a computational biologist at Harvard University and Broad and co-first author of the study, says the scale of the project hinged on collaboration across institutions.
“By leveraging data from Mass General and Dana-Farber, alongside computational frameworks developed at Broad, we were able to make this study a lot larger,” Haradhvala said. “We thought this was a perfect chance to apply single-cell sequencing technologies to understand the actual mechanisms of treatment failure and success in patients.”
Haradhvala worked with study co-first authors Mark Leick (Mass General), Katie Maurer (Dana-Farber), and Satyen Gohil (Dana-Farber/Broad), as well as Gad Getz, a co-senior author, institute member at Broad and professor of pathology at Harvard Medical School, and physician-scientists Catherine Wu, expert in anti-tumor immunity, and Marcela Maus, expert in CAR-T cells. Maus is an associate member at the Broad, associate professor of medicine at Harvard Medical School, and director of cellular immunotherapy at Mass General.
“This was a unique opportunity because we were able to get really deep into the expression profile of the T cells over time,” said Maus. “We wanted to learn which T cells are mediating the response and resistance, because this therapy is a living drug and changes over time. Also, knowing which kinds of the T cells are the most potent helps us design the next generation of T cell therapies.”
Tracking T cells
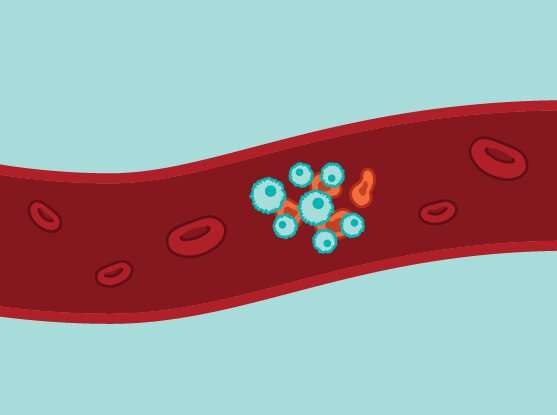
In CAR-T cell therapy, doctors first collect a sample of a patient’s T cells. In the lab, scientists genetically engineer those cells to produce specialized molecules, called chimeric antigen receptors (CAR), and then doctors infuse the cells back into the patient. The receptors on those cells bind key proteins on the surface of cancer cells, helping the patient’s immune system recognize and attack the tumor and preventing recurrence of cancer over time.
In the study, the researchers compared blood samples from patients who received different CAR-T cell therapies for large cell lymphoma, called “axi-cel” and “tisa-cel,” and the therapies themselves. These were the first CAR-T therapies approved by the FDA, in 2017 and 2018. They both target the CD19 protein on the surface of cancer cells, and have similar success rates in the clinic.
Using single-cell RNA-sequencing, the team studied how the CAR-T cells from the therapies changed over time, from before infusion to the patients’ blood to a week after treatment. They found that the cells had surprisingly different characteristics. Most CAR-T cells in patient blood after tisa-cel therapy originated from a particular variety of T cells that contribute to the immune system’s memory of specific antigens. These T cells were also more abundant in patients who responded well to the therapy compared to those who didn’t. The axi-cel treatment led to a greater mixture of T-cell types.
These signatures gave the team clues about which cells help drive relapse. In patients who did not respond to axi-cel, the therapies showed more of a rare subtype of T cell called regulatory T cells, which typically serve as the brakes of the immune system to prevent autoimmune disorders. When researchers led by Leick in Maus’s lab studied CAR-T regulatory cells (CAR-Tregs) in mice, they found that tumors reappeared if the cells made up just 5 percent of the total CAR-T cells infused back into the animals, for both therapies. This suggests that these CAR-Tregs may turn off the activity of cancer-fighting T cells as well.
Haradhvala says that manufacturers could potentially remove CAR-Tregs from the engineered cells to lower the chance of relapse.
Next, the team will work to find markers that might indicate which patients experience side effects such as neurological symptoms, or cytokine release syndrome, an overreaction of the immune system to immunotherapies.
Source: Read Full Article