
Modern blood-thinning drugs (known as NOACs) reduce the risk of serious bleeding by up to 45% compared to the traditional drug Waran (warfarin) in the treatment of blood clots in the legs and lungs. All according to a comprehensive and long-term study conducted at the University of Gothenburg.
Blood thinners are among the most commonly prescribed drugs. The pharmaceutical substance warfarin has been used for over fifty years and is most commonly known by the brand name Waran. In recent years, other pharmaceutical substances that prevent blood clots have been launched, including a group of four different blood-thinning drugs known as NOACs (non-vitamin K oral anticoagulants).
Prior to the introduction of NOACs, studies on short-term treatment regimens showed that such treatment reduced the risk of bleeding compared to Waran. This has resulted in an increasing number of patients who have had a blood clot in the lung or the leg receiving lifelong treatment with this new type of blood thinner.
Extensive Swedish study
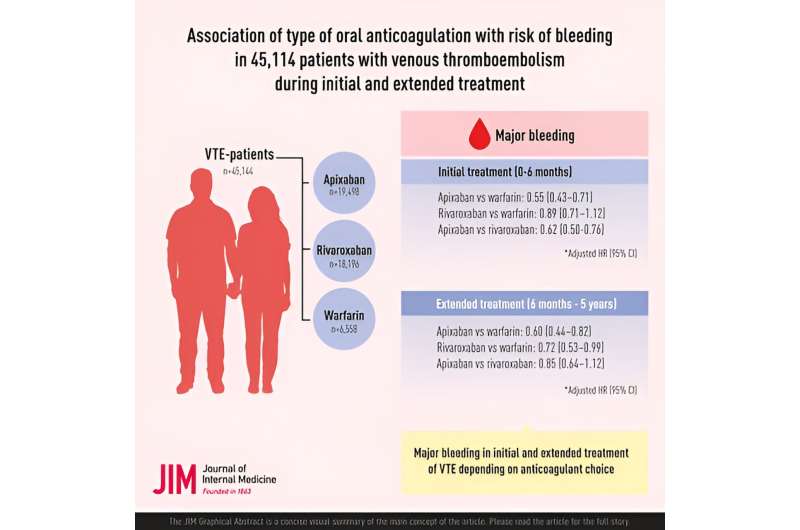
For the first time, researchers have now examined the risk of bleeding in both short-term and extended treatment of blood clots in the legs and lungs in a nationwide study in Sweden. The study demonstrates the advantages of NOACs, in particular the substance apixaban, which is marketed under the brand name Eliquis. The study shows that the risk of serious bleeding is 45% lower with apixaban compared to warfarin.
The study’s lead author, Katarina Glise Sandblad, is a doctoral student at Sahlgrenska Academy at the University of Gothenburg as well as a specialist doctor at Sahlgrenska University Hospital. The results of the study are published in the Journal of Internal Medicine.
“We see that apixaban is associated with a lower risk of bleeding in both the short and the long term compared to warfarin. The short-term risk of bleeding is also lower compared to rivaroxaban (Xarelto), another pharmaceutical substance in the NOAC family. The difference between the different drugs is greatest during the initial months of treatment,” says Sandblad.
Small number prescribed Waran
The study is registry-based, encompassing 45,000 patients who took blood-thinning drugs to treat blood clots in the legs or lungs between 2014 and 2020. Of these patients, most were prescribed drugs in the NOAC group: 43% were prescribed apixaban and 40% were prescribed rivaroxaban. Just under 15% were prescribed warfarin. A few were treated with dabigatran (Pradaxa) or edoxaban (Lixiana). The researchers note that the patients prescribed Waran were, on average, older and more likely to have multiple health conditions, which was taken into account in the analyses.
In conclusion, the study shows that apixaban was associated with the lowest risk of bleeding during the first six months of treatment. Rivaroxaban also had a lower risk of bleeding than warfarin, although not as low as apixaban. The difference between apixaban and rivaroxaban was not statistically significant in extended treatment as both of these pharmaceutical substances were associated with a relatively low risk of bleeding (around 1% per year).
Some patients need Waran
Although warfarin is prescribed increasingly less, Waran still has a certain role to play as an anticoagulant.
“Today, if a patient is prescribed Waran for the first time by their doctor, in the vast majority of cases it is for good reason, although it can be a good idea for the patient to ask about that reason. This applies to patients with atrial fibrillation as well as those with blood clots in the legs and lungs. Patients who are breastfeeding, or who have a mechanical heart valve or a disorder that disrupts the blood’s ability to coagulate, may need to take Waran instead, but many others could switch to a NOAC,” says Sandblad.
More information:
Katarina Glise Sandblad et al, Association of type of oral anticoagulation with risk of bleeding in 45,114 patients with venous thromboembolism during initial and extended treatment—A nationwide register‐based study, Journal of Internal Medicine (2023). DOI: 10.1111/joim.13712
Journal information:
Journal of Internal Medicine
Source: Read Full Article