
Jess Jones, a licensed clinical social worker, treats a number of patients with ketamine-assisted therapy—where clients take ketamine, prescribed by a psychiatrist, in a series of sessions to treat severe depression or other serious mental health issues.
Interest in psychedelic-assisted therapies such as these is growing in the United States, and an emerging body of research suggests that ketamine can successfully treat depression that’s resistant to more traditional methods of treatment. Some states are moving toward legalizing psychedelics: Colorado and Oregon have decriminalized psychedelic mushrooms.
In this Q&A, lightly edited for brevity and clarity, Jones walks through her process of ketamine-assisted therapy, and how she counsels patients who need it. (Jones is also working on clinical research trials involving therapy with other psychedelic drugs, but here is speaking only about her personal therapy practice, which isn’t the subject of research.)
How do patients find you, and what parameters do you set for treatment?
I have information on my website, and then I have a screening form when people reach out for a consultation. It’s a short-term, intensive bit of work, that might last one to three months, roughly, and it’s important patients have ongoing care—from a therapist, spiritual counselor, or support group.
I will gather enough baseline medical information to pass it to one to one of my colleagues who is a psychiatrist to see if there are any red flags—for example, if there’s no point in their doing an evaluation, because of medication they’re on. Then they get a prescription in hand and they come and take the medicine [at my practice].
How do you prepare clients for ketamine-assisted therapy?
My goal is to get to know them as quickly as possible. I ask them to lead me through a series of questions envisioning the future—helping them shift to a place of openness and curiosity.
People come in with different familiarities with non-ordinary states of consciousness. I am primarily a trauma therapist, so I try to help clients feel agency and choice around this decision, to start to tap into things they’ve been defending against. We talk about the different physical senses—they might lose a sense of their body, some people feel numbness or heat, or a really pleasant sensation. We practice putting eye shades on, practice putting music on, and practice having their needs met during a session—like asking for a hand to hold.
What happens during a session?
For the first 15 minutes, we work on getting into an open, receptive state. With some people, it’s letting defensive, protective parts of yourself soften and step back. With others, it’s about reviewing the skills we talked about in prep sessions.
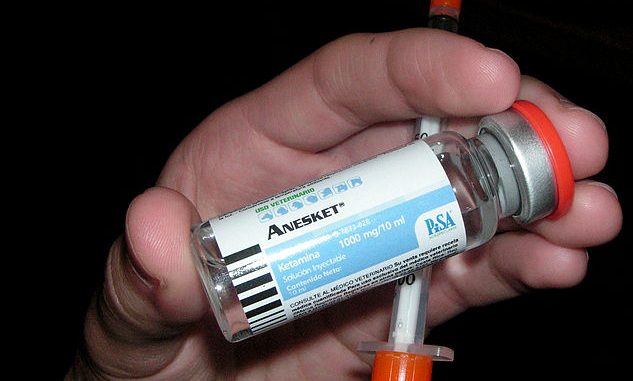
I can’t administer the medicine myself. I’m working with ketamine in a lozenge form—people will put the lozenge in their mouth and swish it around—the ketamine absorbs through your mucosal membranes. Then they put their eyeshades on, their headphones on, and they’re off.
With people on a lower dose, you’re engaging in more therapy—they might come out and talk to you. It’s more about softening defenses. Other times, they’re having a journey, and I can check in on them once an hour.
When they come out, after about 3 to 3 1/2 hours, we’re doing therapy right then in the moment. We won’t revisit trauma, but focus on the good—what pleasant sensations are you feeling, and how can we implant those? Can we, right now, with this fresh coat of snow in your brain, chart new paths?
Then they eat a snack and I send them on their way with a responsible adult. I rarely let people take Ubers, and definitely not after the first journey.
What are follow-up sessions like?
I try to meet with them within 48 hours—that’s recommended by some research, in terms of neuroplasticity. We practice things they’ve learned, and process what’s going on.
We’ll do different types of breath work and talk about healthy emotional containment—how they can start to let themselves experience memories and emotions without medicine, in a safe, contained way.
You’re committed to do this work for a month or so, so I also ask about how it’s going in your daily life.
How do patients pay for this treatment?
Access and equity are important to me—I’m in the credentialing process with Community Behavioral Health [the city agency that oversees Medicaid recipients] here in Philly. I’m credentialed with Quest and Independence Blue Cross. I’m going to have a client soon whose insurance I accept. I can bill for the intake, and prep sessions, and at least an hour of the dosing session—that can just be billed as regular therapy, so a patient would owe a co-pay.
That can bring down costs. I also applied to a foundation called Thank You Life where a clinic can get funds and grants for clients. It won’t start until the spring, but ideally, when we have this grant, it will all be covered for patients, from the psychiatric consultation to the therapy sessions.
Currently, I charge $100 an hour, and $75 an hour for Black and indigenous people of color and folks who are transitioning genders. My psychiatrist’s baseline is $400 for evaluation and $125 for follow-ups. He doesn’t take insurance.
2022 The Philadelphia Inquirer, LLC.
Distributed by Tribune Content Agency, LLC.
Source: Read Full Article