In a recent study published in Thrombosis Research, researchers determined plasma signatures of proteins related to or derived from platelets in acute isolated pulmonary embolism (iPE) and deep vein thrombosis-associated PE (DVT-PE), compared to isolated DVT (iDVT).
Background
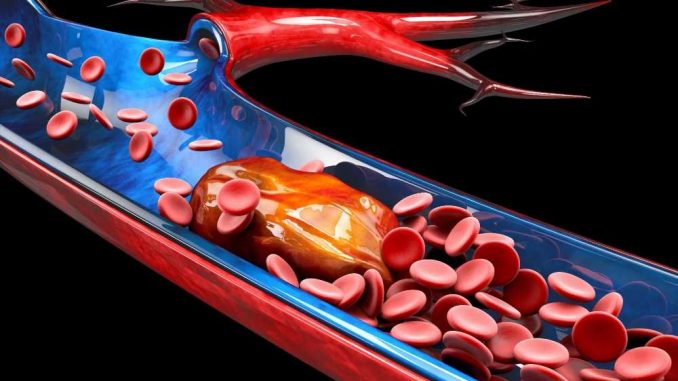
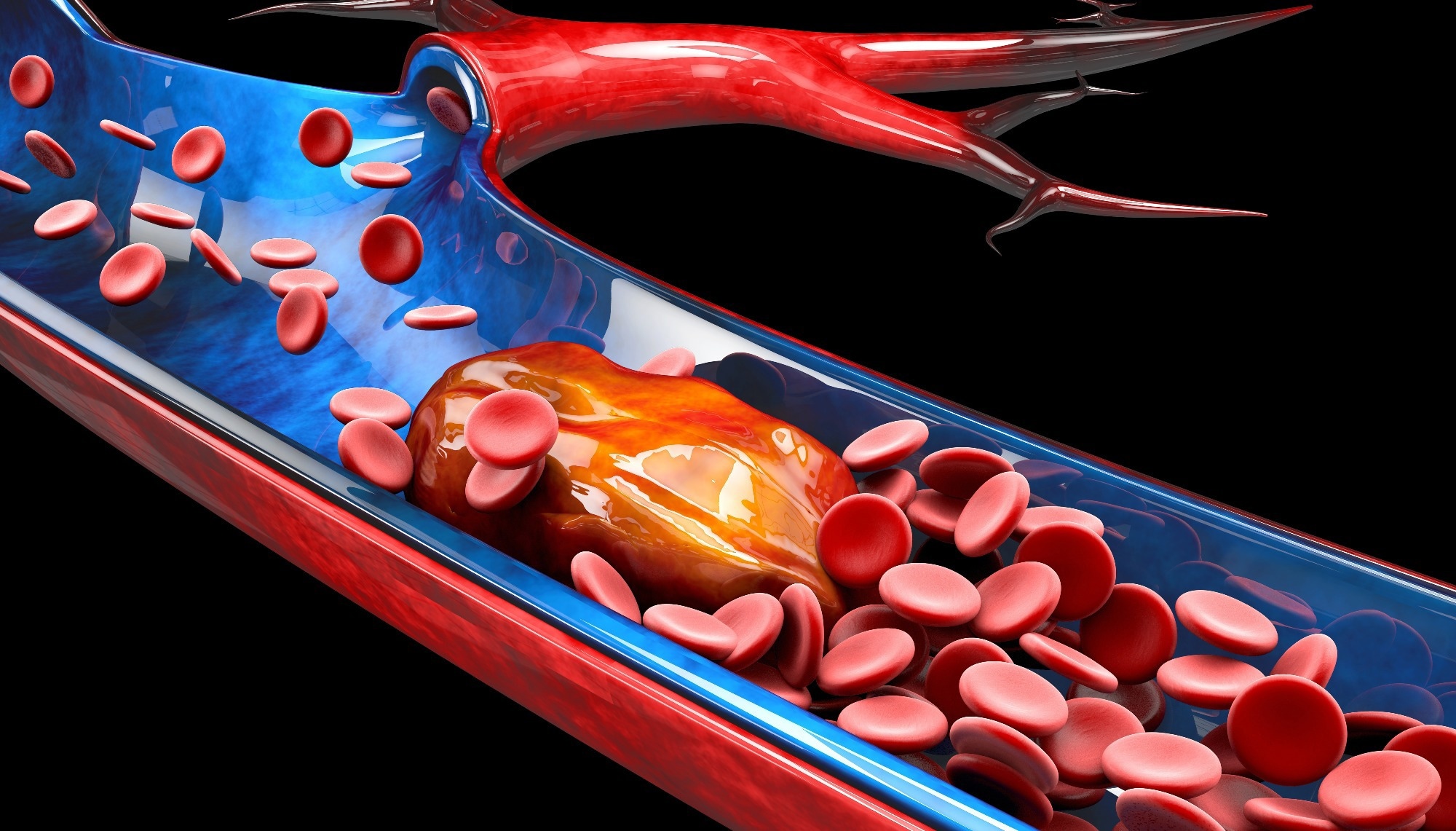
The two primary subtypes of PE are iPE and DVT-PE, and studies have shown that plasma protein profiles for both these conditions differ. Platelets act as cellular linkers facilitating inflammatory crosstalk between immune and endothelial cells at high arterial shear stress. This process is a direct receptor-mediated interaction involving pro-inflammatory molecules and extracellular vesicles (EV). However, local inflammatory responses at the endothelium at low shear stress activate platelets to initiate the development of venous thromboembolism (VTE) and its subtypes, including PE and DVT. The mechanisms governing this process are less well understood.
Experimental data suggest that platelets contribute to thromboinflammation in the venous system by triggering inflammatory and coagulation processes. For instance, using the murine model of VTE, researchers have shown that platelets interact with von Willebrand factor (VWF)-exposing endothelial cells and forming conjugates with leukocytes via glycoprotein (GP) Ibα, as well as triggering endothelial recruitment and leukocyte-dependent coagulation.
Human experiments have shown differential platelet activation and reactivity properties in acute VTE. For instance, platelets from acute VTE patients exhibited more exocytosis of dense granules and lysosomes. It accompanied higher plasma levels of thromboxane B2 but less platelet-dependent thrombin generation than patients with excluded VTE, independent of aspirin therapy.
Mass spectrometry (MS) studies have revealed over 3700 proteins in resting, inhibited, and activated highly purified human platelets. Advanced enzyme-linked immunosorbent assay (ELISA)-based assays with MS could enable qualitative assessment of platelet-released proteins in plasma and isolated platelets. Yet, a more detailed analysis of platelet-associated plasma proteins in large VTE cohorts is missing.
About the study
In the present multicenter prospective cohort study, researchers profiled plasma collected from 541 VTE patients using machine learning-based analysis. The aim was to identify plasma protein signatures for the putative platelet releasate, specific for iPE and DVT-PE. These patients had acute VTE at the time of enrollment, as diagnosed by imaging. While there were 99 iPE patients, 282 were DVT-PE patients, and the team compared their data with 160 iDVT patients. The team used whole-leg color Doppler ultrasonography and computer tomographic (CT) pulmonary angiography for DVT and PE diagnoses. Certified angiologists and radiologists adjudicated and validated all study diagnoses.
They collected study samples as part of the Genotyping and Molecular Phenotyping of Venous Thromboembolism (GMP-VTE) project undertaken in Germany. The researchers used proximity extension assay (PEA) technology for high and low abundant plasma proteins profiling from samples stored at -80°C. PEA fetched normalized expression (NPX) values for all tested plasma proteins integrating oligonucleotide-labeled antibodies and quantitative real-time polymerase chain reaction (PCR) amplification.
The assay panel comprised 444 proteins identified from five databases [e.g., Kyoto Encyclopedia of Genes and Genomes (KEGG) and Gene Set Enrichment Analysis (GSEA) databases]. After comparing, the team finally identified 135 platelet-related proteins in the five PEA panels for further analysis.
Study findings
The study cohort demonstrated a higher prevalence of arterial hypertension, diabetes, and chronic inflammatory, atherosclerotic and cardiovascular diseases in iPE and DVT-PE compared to iDVT. The higher levels of C-reactive protein (CRP), troponin I, and N-terminal (NT)-prohormone B-type natriuretic peptide (NT-proBNP) similarly reflected the greater cardiovascular burden in PE subtypes.
Medication prescription patterns differed accordingly. For instance, antiplatelet therapy, i.e., acetylsalicylic acid (ASA) and clopidogrel, were overrepresented among PE patients. One explanation is that prophylactic antiplatelet medication is prescribed due to suspicion of myocardial infarction in acute PE patients. It is also possible that varying platelet activity exists between PE and iDVT patients because the proportion of antiplatelet agents is higher in the PE groups.
The machine learning analysis of 135 extracted platelet proteins by the Least Absolute Shrinkage and Selection Operator (LASSO)-regularized logistic regression models selected 24% and 22% for iPE and DVT-PE, respectively, which reflected varying protein profiles compared to iDVT. Notably, all 135 platelet proteins demonstrated good association with six platelet activation markers, supporting their likely platelet origin in the plasma of acute PE patients compared to iDVT patients, analyzed via the PEA panels. In contrast to iPE, stromal cell-derived factor 1alpha (SDF-1α) was highly expressed in DVT-PE than in iDVT patients, indicating a potentially distinct role in vascular inflammation and atherogenesis.
In iPE, the protein-protein interaction (PPI) network analysis resulted in four clusters of up to six functionally interacting proteins based on 22 specifically expressed platelet-related proteins compared to iDVT. The main cluster was linked to adhesive, pattern recognition, and immune receptor signaling. These covered the Src family kinases (SFK) c-Src, which transfer ligand signaling via the immunoreceptor tyrosine-based activation motif (ITAM)-associated platelet receptors (e.g., glycoprotein VI [GPVI]).
Relative to iPE, DVT-PE presented one cluster of nine directly interacting plasma proteins related to platelets involved in tissue remodeling and leukocyte trafficking. The tissue inhibitors of matrix metalloproteinases 1 (TIMP1) and TIMP4, prominent effectors of tissue remodeling, were more highly expressed in DVT-PE than in iDVT and were secreted from platelet α-granules.
The authors noted that higher plasma levels of both tissue inhibitors of TIMP1 and TIMP4 were associated with type 2 diabetes, arterial hypertension, and myocardial infarction, which is in line with the higher prevalence of major cardiovascular events in DVT-PE than in iDVT.
Conclusions
The current study results revealed that both PE subtypes presented specific plasma protein profiles associated with platelets. For instance, the study differentiated a higher expression of P-selectin in the plasma from DVT-PE patients compared to iDVT, suggesting a relation with DVT disease severity. Interestingly, thrombin peak height and spontaneous platelet aggregation in platelet-rich plasma were negatively linked in iPE compared to the iDVT phenotype. These results suggested that lower platelet reactivity in vitro might be associated with higher platelet activation in vivo during the acute phase of PE compared to iDVT. More importantly, these results suggested that although PE subtypes share some common but also exhibit different platelet activation patterns.
This study did not address the quantification and characterization of EV in the plasma of VTE phenotypes. In cancer patients, VTE might be linked to increased plasma levels of microparticles. However, in non-cancer patients, a significant increase in platelet-derived microparticles was only observed with recurrent VTE compared to healthy blood donors. Future studies should elucidate the distribution of EV in the different VTE phenotypes. Additional studies are also needed to specify the impact of different cell types on the release of platelet-derived proteins in PE.
In conclusion, the study data indicated that iPE and DVT-PE exhibited specific but varying plasma signatures involved in platelet-related immunothrombosis and thromboinflammatory processes compared to iDVT. Moreover, platelet activation protein profiles appeared to differ between PE subtypes, with a preponderance of secreted proteins in DVT-PE compared to proteins more likely to be released into plasma by EV in iPE. Overall, platelets contribute to regulating distinct plasma protein levels in the acute phase of PE differing between PE subtypes.
- Gaukhar Baidildinova, Vincent ten Cate, Markus Nagler, et al. (2022). Subtype-specific plasma signatures of platelet-related protein releasate in acute pulmonary embolism. Thrombosis Research. doi: https://doi.org/10.1016/j.thromres.2022.10.005 https://www.sciencedirect.com/science/article/abs/pii/S0049384822004157
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: Angiography, Antibodies, Aspirin, Assay, Blood, Cancer, Cell, Chronic, Clopidogrel, C-Reactive Protein, CT, Deep Vein Thrombosis, Diabetes, ELISA, Embolism, Enzyme, Gene, Genes, Genotyping, Glycoprotein, Imaging, in vitro, in vivo, Inflammation, Leukocyte, Ligand, Lysosomes, Machine Learning, Mass Spectrometry, Microparticles, Myocardial Infarction, Oligonucleotide, Phenotype, Platelet, Platelet-Rich Plasma, Platelets, Polymerase, Polymerase Chain Reaction, Protein, Pulmonary Embolism, Receptor, Research, Spectrometry, Stress, Thromboembolism, Thrombosis, Troponin, Type 2 Diabetes, Tyrosine, Vascular, Venous Thromboembolism

Written by
Neha Mathur
Neha is a digital marketing professional based in Gurugram, India. She has a Master’s degree from the University of Rajasthan with a specialization in Biotechnology in 2008. She has experience in pre-clinical research as part of her research project in The Department of Toxicology at the prestigious Central Drug Research Institute (CDRI), Lucknow, India. She also holds a certification in C++ programming.
Source: Read Full Article