
Cancer mutations often incapacitate critically important genes, forcing tumors to depend heavily on other genes for survival. Such genetic dependencies are attractive targets for new cancer therapies.
In a study published in Cell Reports, scientists from the Cancer Dependency Map (DepMap) project at the Broad Institute of MIT and Harvard and the Dana-Farber Cancer Institute and colleagues report a genetic dependency that could be present in up to one-third of all cancers. In these cancers, the researchers found, one of two related genes, VPS4A and VPS4B, is deactivated, causing the tumors to rely on the other gene for survival. Drugs designed to turn off that other gene could potentially kill those cancers.
In their study, the team used large-scale CRISPR- and RNA interference (RNAi)-based screens of 873 cancer cell lines from more than two dozen forms of cancer, focusing on cancers in which genes called tumor suppressors have been deleted or turned off. Such genes normally prevent damaged cells from growing unchecked.
“Tumor suppressors are hard to target therapeutically,” said Brenton Paolella, a research scientist with the DepMap team and the Broad Cancer Program and Dana-Farber, and co-first author of the study with postdoctoral fellow Jasper Neggers. “But we realized we had an opportunity to find new targets by looking for other genes associated with tumor suppressor loss.”
The researchers turned their attention to VPS4A and VPS4B after examining cell lines that had lost one of two tumor suppressor genes, CDH1 and SMAD4, that are commonly deleted in cancer. They found that VPS4A is often deleted along with CDH1, which sits close by it on chromosome 16. They also discovered a similar relationship between VPS4B with SMAD4, which occupy the same neighborhood on chromosome 18.
Interestingly, the research team noted that cell lines representing a wide variety of cancers relied on one of the two VPS4 genes for their survival, including pediatric rhabdomyosarcoma and bile duct, bladder, breast, colorectal, esophageal, gastric, liver, lung, ovarian, and pancreatic cancers. In total, cell lines representing approximately a third of all cancers harbored a VPS4A or B dependency. For confirmation, they queried data from the Cancer Genome Atlas, finding VSP4B loss in 33 percent of all cancers collected in that project, and VPS4A loss in an additional 27 percent.
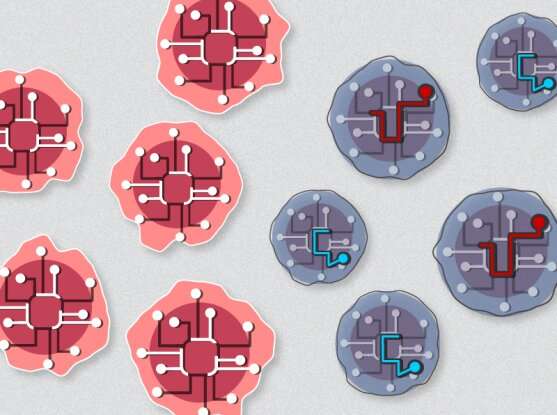
VPS4A and VPS4B are paralogs—molecular fraternal twins that diverged from a common genetic ancestor and share similar tasks. Both encode parts of a molecular machine called the ESCRT complex (which helps maintain the integrity of membranes within and surrounding the cell).
The research team—led by Neggers, Paolella, DepMap assoicate director and institute scientist Francisca Vazquez, and associate member Andrew Aguirre of Broad and Dana-Farber—further explored whether the loss of one VSP4 gene would leave cancer cells dependent on the other. And indeed, in multiple cellular and animal models, they found that cancer cells lacking SMAD4 and VSP4B were vulnerable to VPS4A disruption.
Source: Read Full Article