
When newborn babies or children with heart or lung distress are struggling to survive, doctors often turn to a form of life support that uses artificial lungs. This treatment, called Extracorporeal Membrane Oxygenation (ECMO), has been credited with saving countless lives. But in some cases, it can also lead to long-term brain injury.
Now, a research team led by UT Southwestern scientists has shown that a machine learning program can predict, more accurately than doctors, which babies and children are most likely to suffer brain injury after ECMO. The study was published last month in the Journal of Clinical Medicine.
“Doctors have always had some intuition about who might be at risk, but until now we really haven’t had good data to pinpoint what factors are precipitating brain injury from ECMO,” says study leader Lakshmi Raman, M.D., associate professor of pediatrics at UT Southwestern and a critical care specialist at Children’s Health. “I don’t think we’ll be able to fully eliminate these injuries, but I hope that with better predictions we can mitigate the risk.”
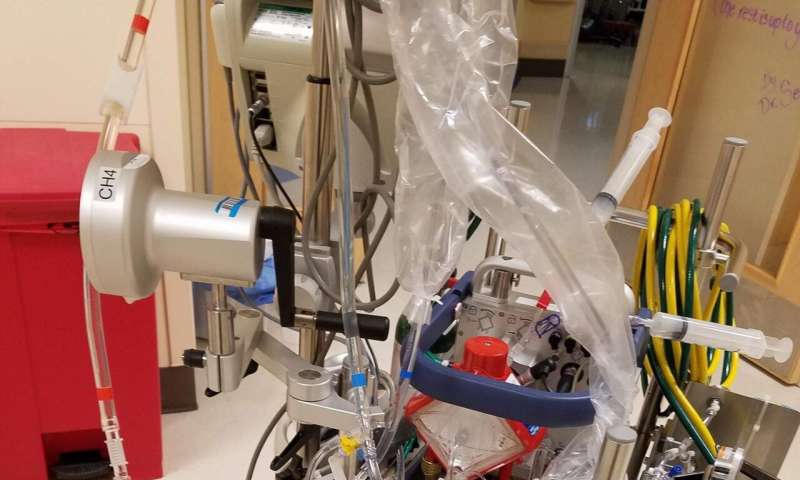
ECMO works by routing blood out of a patient’s body, pumping it through a device that adds oxygen, removes carbon dioxide, and keeps the blood warm before returning it to the body. ECMO is used in both children and adults, but the most frequent patients are newborns. The therapy takes pressure off the heart and lungs while they mature or recover from injury.
Many patients treated with ECMO end up with brain complications, however, and doctors don’t fully understand why. The brain injuries have often been attributed to blood-thinning drugs given during ECMO, but studies have failed to back up that link.
“I became really interested to see whether we could come up with an algorithm that takes all these different factors and tries to identify what predisposes some patients to brain injury,” says Raman.
Raman and her collaborators used data on 174 patients under the age of 18, including 70 babies under 30 days old, who were treated with ECMO at Children’s Medical Center Dallas between 2010 and 2019. In each case, CT or MRI images of the patient’s brain after ECMO was available. Brain injury was detected by a scan in 81, or 51 percent, of the patients.
The researchers entered data on each patient—including age, weight, gender, medications, type of ECMO, primary reason for ECMO, and how long they received ECMO—into a machine learning program called a neural network that is designed to identify patterns in datasets. The program analyzed over 35,000 clinical hours of ECMO treatment and 1.4 million data points across 35 variables.
The resulting model had a 73 percent sensitivity rate of predicting brain injury after ECMO and 80 percent specificity rate. This beat out the prediction power of clinicians, who had suspected brain injury in 61 patients, with a sensitivity of 39 percent and a specificity of 69 percent.
Surprisingly, whether a patient was on anti-coagulant drugs, or the dosage of those drugs, had little effect on brain injury. A patient’s heart rate and blood pressure, however, were found to help the model predict brain damage.
“I think this probably means we need to focus more attention on those blood flow variables,” says Raman. “We’re already starting to do work in that direction.”
Source: Read Full Article